OPTN,
Savior of the Nephrotics
Zhizhuo Zhang Xiao Yuan Yang Su
The OPTN, a savior in the eyes of many diseased, saves and prolongs numerous lives. Although the OPTN is functioning, there are still approximately 95,000 candidates waiting for an organ. The efficiency and effectiveness of the network are in dire need of improvement. Our project demonstrates several solutions to the critical bottleneck in current OPTN system.
We first build a Monte Carlo Simulation model for the OPTN. Our model is convenient and useful for the researchers to attempt new policies, since the model can be easily modified. Through simulating, three potential bottlenecks are discovered:
l Many cadaveric kidneys
can not match patients’ tissue type.
l Many patients reject
the offered kidneys.
l Live willing donors
and patients pairs are not compatible.
To deal with the current statue, some policies are discussed. We also find that implementing the policies of other countries is of little help, due to the different situation.
We use some formulae to estimate the maximal number of patients who can benefit from n-way exchange system, and make a comparison with the simulation results. We discovered 3-way exchange can generate about 10% more matched patients than 2-way in certain population size, while 4-way has a slightly effect on the maximum size.
A strategy is designed for a patient to make the decision before the transplant, by using the risk decision-making methods.
A suggestion is raised to give attention to a fairness and efficiency concerning the political ramifications. We also consider modifying the current policies to decrease the priority of pediatrics for enhancing the interests of the whole society. We definitely forbid organ selling and buying, because of the destruction effect on the whole society.
Nearly all the factors influenced donors are showed in our paper. We believe our recruiting methods will be of dramatic help for the OPTN.
Content
OPTN,
Savior of the Nephrotics
2. The
Restatement of Problems
3. Simulation
of the Transplantation Network
3.7 Investigation of the Policies of another Country
4.5 Integer Programming of N-Way Exchange
4.8 Tissue type incompatibility
5. Political and Ethical Issues
5.1 Political Issues on the Transplant System
5.2 Ethical Issues in the Transplant System
5.3 The Discussion of Selling Organs
6.1 Factors Influencing Donation
6.2 The larger the net, the bigger the mesh
6.3 Recommendations of recruiting more altruistic donors
1. Introduction
Organ transplantation is of great significance in saving and prolonging people’s lives. Although science and technology in medicine and health is developing at an increasing rate with dramatic breakthroughs, the demand for organs greatly exceeds the supply. This situation occurs globally. To solve the problems in organ procurement and transplantation, hundreds of countries have developed different systems and policies among which the US is a leading force.
Organ Procurement and Transplantation Network (abbr. OPTN) is established in 1984.It is a private, non-profit organization under federal contract. Its two main goals are to increase the effectiveness and efficiency of organ sharing and equity as well as the supply of donated organs available for transplantation. The United Network for Organ Sharing (abbr. UNOS) administers the OPTN under contract with the Health Resources and Services Administration (abbr. HRSA) of the U.S. Department of Health and Human Services (abbr. HHS). HHS implemented a Final Rule establishing a regulatory framework for the structure and operations of the OPTN.
Thanks to the operation of the network, more and more donors (alive or deceased) are registered and transplantations take place monthly. But the waiting list of candidates becomes longer and longer. The number of candidates on it exceeds 95,000 when we are writing this paper. Many patients in need of organs have to wait a long time. The current system should be improved in order to function better in the future.
We can find the latest policies of organ transplantation on the OPTN website, which are changing annually to match the ongoing complexities. Experts at UNOS have done lots of researches on the organ matching process. It is a pity that the network is far from perfect. Scores of problems are discovered, such as bottleneck in the network and lack of recourse. Transplantation policies in countries other than the US are also investigated. By comparison, a better procedure may be found to improve the current network.
Our investigation focuses on the kidney transplantation. Kidney plays a significant role in the human body. In the US today, patients are waiting for healthy kidneys while the amount of kidneys available each year is between 15,000 and 16,000. The average waiting time is approximately three years, too long for some neediest patients to survive. Patients who are at the end stage of kidney disease may pay for an expensive dialysis or do a kidney transplantation surgery. Worse still, they may die without either. Even if they can get a kidney from the cadaver queue, they may give it up to wait for a better one. During transplantation, various issues need to be considered, such as the physical and psychological conditions of the recipients and the donors. The compatibleness of ABO blood type and the matches on HLA markers in the blood are two key factors of the success of survival of the transplant. In order to maximize the survival rate after transplantation, mismatches of HLA makers should be minimized. It is common that people want to donate kidneys to their relatives or friends. However, the blood type or the HLA mismatches may render them helpless. New policies and procedures should be made to increase the amount of successful transplantation.
The kidney exchange system in Korea can be used to solve the problem that most original donor-recipient pairs don’t match. Three ideas of the exchange system are paired-kidney donation, list paired donation and n-paired donation.
There are various kinds of issues referred to organ transplantation. We must concern almost all fields in this topic and balance all dimensions.
Several criteria and policies are developed according to ethical concerns. Whether a patient should go on to the waiting list or come off mainly depends on his/her physical situation. For example, patients with a malignant disease like AIDS have to be excluded from the list. Criteria to determine priority like the time on the list are also made, which include the time on the list, the quality of match between donor and recipient, and the distance between donor and recipient. A recent change of policies made by the UNOS gives higher priority to children under 18 years old. Some say that it is a squander to transplant kidneys to older recipients, since old age means lower survival rate after transplantation. The priority on different ages is inevitably debated.
Not only the ethical issues, but also the political issues are produced. If two persons are both in urgent need of kidneys, but there is only one available; where should it go? Can a drug dealer obtain kidney transplantation? Nowadays, transplants are usually performed in a few large centers in big cities, by a few experienced experts and surgeons. Doctors in small communities lose the chance to do them, which is an indispensable experience. Would there be a fair system to deal with this problem?
Another hot topic discussed by the public is the trading and solicitation of organs, which is forbidden in the US. However, some agencies advocate donors to receive financial compensation. ”Presumed consent” assumes everyone to be an potential organ
donor.
2. The Restatement of Problems
There are 6 tasks presented to be completed in our paper, each from different aspects. We list the 6 tasks concisely as follows.
l Build a math model for the US transplant network, considering the questions: where are the bottlenecks for efficient organ matching? Where and how could the additional resource be used for improving the efficiency? Would the network function better if divided into smaller ones? Can the network be more effective by saving and prolonging more lives? Suggest the policies changes and modify the model.
l Modify the model to investigate the transplantation policies in another country and determine if the policies in the US would be improved by implementing the procedures in the country. Write a one-page report to Congress, addressing the issues in the last task and the information and possible improvements from the research of the different country’s policies.
l Devise a procedure to maximize the number and quality of exchanges, taking into account the medical and psychological dynamics of the situation. Justify in what way the procedure achieves a maximum. Estimate how many more annual transplants will generate, and the effect on the waiting list.
l Devise a strategy for a patient to decide whether to take an offered kidney, or to participate in a kidney exchange. Consider the risks, alternatives, and probabilities in your analysis.
l Discuss the recommendation of changes to current criteria and policies, ethical dimensions of the exchange procedure and the recommended patient strategy in the last two tasks. Rank order the criteria used for priority and placement with rationale. Consider the problem of allowing people to sell organs for transplantation. Write a one-page paper to the Director of the US Health Resources and Services Administration.
l Answer the questions: How do the risks and others affect the decision of the donor? How do perceived risks and personal issues influence the decision to donate? Does the size n of the n-paired network have any effect on the decision of the potential donor, if entering a list pair network? Modify the model to reflect and analyze these issues. Suggest ways to develop and recruit more altruistic donors.
3. Simulation of the Transplantation Network
Prior to model construction, we read some literatures about the network of some scientists and researchers. We find that most of the literatures utilize the simulating method to investigate the operation of the network. A famous software tool named UKAM, which stands for UNOS Kidney Allocation Model, is developed for the simulation and analysis of national kidney allocation policies. During our investigation, we also adopt the simulating method to build our model.
First, we obtain the transplantation data from the OPTN website. The UNOS annual data reports provide us sufficient data, including the organs, the waiting list, the donors, so on and so forth. The data are often categorized. Various kinds of information can be found, such as age, sex, ethnicity, blood type, etc. Since our research focus on the kidney transplantation, we utilize data related to kidney as a base to construct our model.
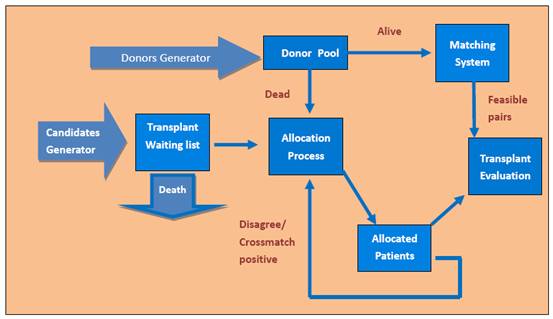
We consider the nation as a whole when
building the model, involving all the data from different regions. By using the
Figure
1
3.1 Candidates Generator
Since we do not have the detailed data of each real patient, we generate virtual ones according to the historical data in Candidates Generator Component. A patient has dozens of attributes, such as age, race, gender, blood type. What we know is the distribution of a specific type in each attribute. To make an example, all the attributions are taken as independents and a candidate is generated randomly according to the distribution of each attribution in UNOS 2006 Data. Further more, the model assumes that new patients arrived according to Poisson process, of which the arrival rate is increasing annually. After candidates join the waiting list, they remain until they are offered an allocation, or die. The probability of mortality of each day can be estimated from the data reports.
3.2 Donors Generator
The process of coming of donors is similar to the process of coming of patients. We generate the distribution of donors with different characteristics (including dead or alive) by the methods mentioned above, utilizing the data resource. New donors arrived according to a Poisson process, of which arrival rate is increasing by year as well.The donors stream will store in the donor pool at first. Then the dead donors will go into the allocation system at once, who will be discarded if no candidates accept at that day. On the other side, the living donors and their corresponding patients will be transferred to the matching system. An assumption has been implied here is that all living donors are willing donors who only wish to donate their organs to specific patients (their relatives usually).
3.3 Allocation Process
Once a kidney becomes available, the
allocation begins. We rank the patients on the national waiting list, which is
based on the policies of OPTN. The factors we need to consider comprise of age,
blood type, PRA level, etc. PRA stands for Panel Reactive Antibody (point system
described in table 1). PRA level is measured to reflect the sensitivity to the
donor. If one’s PRA level is too high, it will be difficult for him or her to
discover a suitable kidney. To model transitions from one PRA
levels(0-9,10-79,80+) to another, a Markov matrix was constructed using
historical waiting list data from 1999-2006 and stratified by the time already
spent on the waiting list(0-30 days,31-300 days,301+ days).Based on this
transition matrix, each patient’s PRA value is updated by their waiting time.
Organs are allocated first at the local level, then region, nation finally.
According to the UNOS point system (table 1), each patient in the waiting list
is given a score, reflecting the priority. The kidney is offered to the person
with the highest priority. To determine the likelihood of organ rejection of
the patients, a test called cross match would be done. If the cross match is
negative, the transplantation is performed. Otherwise, the next candidate will
do the cross match. The simple method to simulate the crossmatch procedure is
that the patient’s current PRA value was substituted for the probability of a
positive crossmatch[
Table 1
|
Category |
Points |
|
Waiting time1 |
1 point for each full year on the waiting list |
|
Waiting time2 |
t/max_waiting_time (t is the waiting time of the patient) |
|
Panel reactivity |
4 points for PRA >80% |
|
Pediatric candidates |
4 points when age<11 3 points when 11<age<18 |
|
Blood Type |
Negative Infinite when doesn’t match blood group |
|
Tissue Matching |
2 points for no DR mismatch 1 point for 1 DR mismatch |
3.4 Matching System:
Many living donors only wanted to donate some designated patient who has close relation with them most of the time. As a result, a patient-donor pair has been formed. If they are satisfied with the transplant condition (including blood matching and tissue matching), the pair is known asa compatible pair. Otherwise, the pair is denoted as an incompatible pair. Matching System gives opportunities to incompatible pairs, and this process is called n-way exchange (more detail in task 3).
3.5 Transplant Evaluation
The transplant evaluation component generates the result of each transplant. This component uses PRA value to estimate the survival time of the patient (survival less than one year means graft fail) through the UNOS data of 2006.
After the simulation model for OPTN is built up, we can run it to simulate the reality. Because of lack of time and resources, we simplified our model. But we can investigate the efficiency and effectiveness of the problem by using the model. If the allocation policies are changed, we just need to change the algorithm of organ allocation. By analyzing the output of the model, we can do some research on different policies.
Three bottleneck:
1.
Many cadaveric kidneys can not match patients’ tissue type, even
there are a large number candidates.
2.
Many patients reject the offered kidneys regarding that not good
enough.
3.
Live willing donors and patients pairs are not compatible.
We
dicuss the patient choice bottleneck and kidney pairs matching bottleneck in
the task 4 and task 3. And bottleneck may be released by more resource given.
3.6 More resource require
Many cadaveric kidneys can’t match patients’ tissue type, even there are a large number candidates. That’s the direct cause of what is called repellency. As a fact in medicine, repellency was due to immunoreactions. Presently there are some way to restrain immunoreactions, but putting aside of the cost which is still too expensive, stabilities and long-term effects on immune-system remain unclear. As a matter of fact, it wouldn’t be comfortable for patients to accept the cost of long-term effect on immune-system. Therefore, more resource should be devoted to research the essential mechanism of repellency and the way of avoiding it without any negative long-term effect for this bottleneck in transplantation.
In order to demonstrate the bottleneck1 ,we use the simulation model to reveal the fact. The parameters of generation (candidate and donor) is derive from UNOS data 2006 . And a survival assumption should be stated here.
Assumption : Probability of patient i dying before time t is of negative-exponential distribution. Denoted TDeath(i) as the dying time, the assumption is formally described as
Pr{TDeath(i) < t} = 1 – exp(–λit),
where λi is a fixed positive real number and t in [ 0, +∞ ). As what is cited in theory of probability texts, λi stands for the reciprocal of the expectation of remaining survival time for i th patient. To simplify simulation, we assume all λi are equal. As could be easily discovered, it wouldn’t make a significant difference if we assume λi is a random variable which forms specific distribution because the simulation itself has some kind of random city which has been enough for analysis.
Table 2
|
Candidate |
Donor |
||||
|
Race |
|||||
|
White |
39.35099% |
75.67675% |
|||
|
Black |
34.73558% |
11.36577% |
|||
|
Hispanic |
17.38851% |
10.09098% |
|||
|
Unknown |
0.00143% |
0.20548% |
|||
|
Asian |
6.50872% |
1.70108% |
|||
|
American
Indian/Alaska Native |
1.08741% |
0.29953% |
|||
|
Pacific Islander |
0.67016% |
0.22899% |
|||
|
Multiracial |
0.67302% |
0.43140% |
|||
|
Age |
|||||
|
< 1 Year |
0.00714% |
0.66449% |
|||
|
1-5 Years |
0.16290% |
3.60049% |
|||
|
6-10 Years |
0.20148% |
2.89716% |
|||
|
11-17 Years |
0.69588% |
10.85974% |
|||
|
18-34 Years |
11.57424% |
30.01533% |
|||
|
35-49 Years |
29.92298% |
25.41914% |
|||
|
50-64 Years |
41.74014% |
20.75240% |
|||
|
65 + |
15.71525% |
5.79125% |
|||
|
BloodType |
51.91179% |
||||
|
O |
51.91179% |
30.24697% |
|||
|
A |
30.24697% |
15.03834% |
|||
|
B |
15.03834% |
2.80396% |
|||
|
AB |
2.80396% |
||||
|
Candidate PRA |
DonorType |
||||
|
0-9% |
67.30000% |
Cadaveric |
54.97328% |
||
|
10-79% |
21.20000% |
Living |
45.02672% |
||
|
80+% |
15.10000% |
||||
The resource is mainly immunoreactions-suppression drugs, which can
increase the probability of allocation no matter how the tissue matching. The
parameter ![]() is descried the drugs
influence of negative of cross match. For example, the origin negative
probability is 0.15 and
is descried the drugs
influence of negative of cross match. For example, the origin negative
probability is 0.15 and ![]() =2 , then the real negative probability
is 0.3. The simulation result are shown Table3, the wastage rate is described
as the ratio of kidney discarded. The lower wastage rate, the more efficient
the network works.
=2 , then the real negative probability
is 0.3. The simulation result are shown Table3, the wastage rate is described
as the ratio of kidney discarded. The lower wastage rate, the more efficient
the network works.
Table 3 The comparison result of the simulation from 2006 to 2015
|
|
Current |
|
|||||
|
|
Mean waitTime |
Mean QueueLength |
Wastage kidneyRate |
meanwaittime |
Mean QueueLength |
Wastage kidneyRate |
|
|
06 |
1025.76148 |
73887.25 |
0.27316542 |
953.2252 |
68481.0925 |
0.11830431 |
|
|
07 |
1150.04450 |
41854 |
0.25160372 |
1036.904662 |
39786.7175 |
0.19599774 |
|
|
08 |
1282.83783 |
31901.13889 |
0.28108793 |
1078.087317 |
31178.3275 |
0.21300880 |
|
|
09 |
1402.42273 |
26523.95833 |
0.29720882 |
1175.956023 |
27118.93563 |
0.22055670 |
|
|
10 |
1454.49925 |
23195.38333 |
0.41638664 |
1153.380303 |
24916.3895 |
0.21305630 |
|
|
11 |
1391.96141 |
21191.72222 |
0.28366120 |
1131.40098 |
22783.8375 |
0.1871949 |
|
|
12 |
1413.28717 |
19754.84524 |
0.3657170 |
1173.85603 |
21615.525 |
0.24713686 |
|
|
13 |
1422.13345 |
18616.88542 |
0.3661718 |
1172.493738 |
20882.27813 |
0.23428819 |
|
|
14 |
1445.03673 |
17932.80556 |
0.3966860 |
1180.207481 |
19888.11028 |
0.15231113 |
|
|
15 |
1524.64079 |
17564.23333 |
0.3883412 |
1167.123594 |
19354.3385 |
0.23144829 |
|
Figure 2 wastage rate comparison from 2006 to 2015
3.7 Investigation of the Policies of another Country
We select the transplantation policies in
3.8 Reports to Congress
We construct a Monte Carlo Simulation model
for the research of the
The potential bottlenecks are found after simulation, which we list as follow:
l Many cadaver kidneys can not match patients’ tissue type, even there are a large number candidates.
l Many patients reject the offered kidneys regarding that not good enough.
l Live willing donors and patients pairs are not compatible.
Since cadaver kidneys can be preserved for just a short period, if we cannot find suitable recipients for them, they have to be discarded, leading to a huge waste of the scarce cadaver kidneys. On the other hand, patients may reject an offered kidney to purse a better one. Moreover, many intended donors and patients pairs are incompatible in blood type or tissue match. To solve these problems, we can design a strategy for the patient choice and encourage organ exchange among incompatible pairs.
If more medical resource is available, we can use them before the transplant surgeons. Some medicines have been invented to restrain the effect of HLA mismatch. Using these medicines, the pain of recipients can be alleviated and the survival rate is increased.
Dividing the national network into smaller ones such as at the region or state level will weaken the function of the OPTN. Since the connections among regions are severed, candidates are not able to receive donors from other regions.
Saving and prolonging more lives would definitely enhance the effectiveness of the system. Meanwhile, the kidneys are saved since fewer patients need to accept a second transplant due to the failure of the last one.
At last, we do not recommend investigating
the policies of other countries. Because the situations vary from countries to
countries, a policy which works well in one place may not suit for another one.
We consider there is little worth to consult to policies outside of the
4. Kidney Exchange System
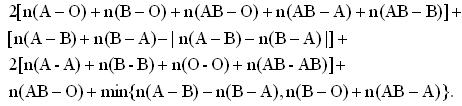
Before we devise a procedure of kidney exchange, it is necessary to introduce the idea about donor exchange. The most often exchange is paired-kidney donation. Suppose that donor 1 want to give his kidney to recipient 1. But I am afraid to say that their blood types are not compatible, since donor 1 has blood type A, while recipient 1 has blood type B. There is another pair facing the same problem. Donor 2 has blood type B, but recipient 2 has blood type A. If each donor donates to the other recipient, two new pairs are created, both of which have compatible blood type. The surgery usually is operated in the same place and on the same day. Not only the exchange can take place between two living pairs, but also it can take place in the cadaver queue, which is called as list paired donation. A donor donates to another patient waiting for a cadaver kidney. The original patient of the donor obtains a higher priority to receive a kidney from the cadaver queue in return. Moreover, the paired-kidney donation, or the 2-way donation, can be expanded to 3-way, 4-way, even n-way. Since many original donor-recipient pairs are incompatible in the blood type, the exchange system will be of great help to save patients’ lives.
Figure 3 The compatibility of different blood type
4.1 N-Way Exchange Model
We continue utilizing the Monte-Carlo simulation method to analyze the problem in Task 3. First of all, we try to gain some theoretical conclusion. Our goal is to derive the expressions for the maximum umber of patients, who can benefit from a feasible set of kidney exchanges among a large population of incompatible pairs. We assume that a positive cross match does not occur, in order to simplify the problem. We use X-Y to denote a patient-donor pair, where X, Y can be A, B, AB and O, the blood type of the patient and the donor. n(X-Y) denotes the number of pairs who have the blood type X-Y. Noticing that pairs of type O-A, O-B, O-AB, A-AB, and B-AB occur more frequently since the kidneys they offer is in lower demand than the ones they need. Therefore, we assume that at least one pair of each type remains unmatched in the exchange.
4.2 2-Way Exchange
We can calculate the maximum number of matched patients with only2-way exchange on the base of the assumptions and the general knowledge of blood type compatibleness. The maximum number is:
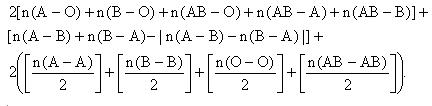 (1)
(1)
In the formula above, [n] means the greatest integer not larger than n.
4.3 3-Way Exchange
Obviously, allowing 3-way exchange will create more matched pairs. To simplify the expression of the maximum number, we assume that n(A-B)>n(B-A), and there is either no X-X pair or there are at least two of them. The maximum number of patients who can be matched with 2-way and 3-way exchanges is:
 (2)
(2)
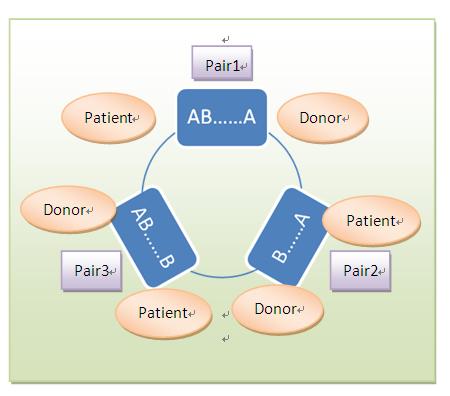
Figure 4 a sample of 3-way exchange
4.4 4-Way Exchange
Similarly, the maximum number of patients who can be matched with 2-way, 3-way and 4-way exchanges is
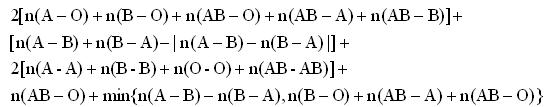 (3)
(3)
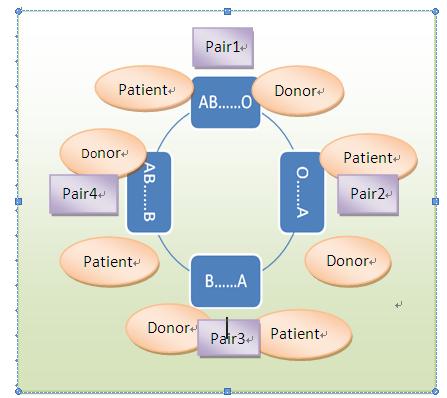
Figure 5 a sample of 4-way exchange
4.5 Integer Programming of N-Way Exchange
We construct an IP model to predict the exchange problem. Let N denotes the amount of patient-donor pairs. Patient is denoted by Pi, and donor is denoted by Dj. Let C be the compatible matrix and X be the acceptance matrix. If is Pi compatible with Dj, cij=1, else cij=0. If Pi receive a kidney from Dj, xij=1, else xij=0. The IP is as follows.
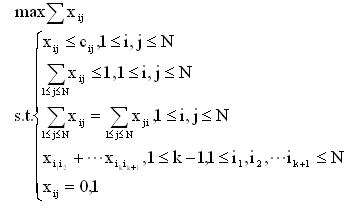 (4)
(4)
Solving the IP in Lingo, we can obtain the maximal set of patients who can benefit from any way exchange.
4.6 Simulating the Model
During simulation, we will consider the tissue type incompatibilities. We can compare the result to the one under the assumption that exchange was limited only by blood type. We not only compute the actual maximal number of exchanges, but also compute the predicted (upper bound) number based on the formulas derived above. It is surprised that the formulas predict the actual number of exchanges very well. That is, the upper bounds on the maximal number of exchanges when exchange is limited only by blood type incompatibility are not far from the actually numbers of exchanges. Moreover, exchanges which are more that four pairs contribute just a little to the efficiency.
4.7 Generate the Pairs
The characteristics such as the blood-types of patients and donors, the PRA distribution of the patients, donor relation of patients, and the gender of the patients are generated using the empirical distributions of the OPTN annual data report. In our simulations, we randomly generate a series of patient-donor pairs using the population characteristics explained above. Only when the patient-donor pair are either blood-type or tissue-type incompatible do we keep them, while the compatible intended pair are excluded. This process goes on till we obtain a sample with the expected size.
4.8 Tissue type incompatibility
Tissue type incompatibility (a positive cross match) is independent of blood type incompatibility. Patients in the OPTN database are divided into the following three groups based on the chance that they may have a cross match with a random donor:
1. Low PRA patients: Patients who have a positive cross match with less than 10 percent of the population.
2. Medium PRA patients: Patients who have a positive cross match with 10-80 percent of the population.
3. High PRA patients: Patients who have a positive cross match with more than 80 percent of the population.
More detailed PRA distribution being unavailable in the medical literature, we simply assume that:
1. Each low PRA patient has a positive cross match probability of 5 percent with a random donor;
2. Each medium PRA patient has a positive cross match probability of 45 percent with a random donor;
3. Each high PRA patient has a positive cross match probability of 90 percent with a random donor.
4.9 Simulations Outlines
For each sample of incompatible patient-donor pairs, we find the maximum number of patients who can benefit from an exchange when both blood-type and tissue-type incompatibilities are considered. The different ways of exchange we considered are list below:
1. No exchange is allowed.
1. Only 2-way exchanges are allowed.
2. 2-way and 3-way exchanges are allowed.
3. 2-way, 3-way, and 4-way exchanges are allowed.
4. Any size exchange is allowed.
To find the maximal number of patients who can benefit from an exchange, we use integer programming techniques. We compare these numbers with those implied by the expressions mentioned above in order to see how well the formulae can estimate the actual number.
Since many high PRA patients cannot be part of any exchange due to positive cross match, we calculate two sets of upper bounds induced by the formulae we developed.
Upper bound 1 is the maximal exchange size developed by the formulae. Upper bound 2 reports the average over all populations for the formulas using the smaller population of incompatible patient-donor pairs. Upper bound 2 provides a more precise upper bound to the number of exchanges that can be found. The fact that the difference between the two upper bounds diminishes as the population size increases, which reflects that, in larger populations, even highly sensitized patients are likely to find a compatible donor.
The percentages of matched patients on different way are listed below.
Table 4
|
Size |
Method |
1-way (%) |
2-way (%) |
3-way (%) |
4-way (%) |
n-way (%) |
|
25 |
Upper bound 1 |
|
39.3 |
47.7 |
50.1 |
|
|
Upper bound 2 |
|
36.7 |
46.5 |
48.2 |
|
|
|
Simulation |
17.2 |
35.4 |
45.1 |
47.3 |
48.0 |
|
|
50 |
Upper bound 1 |
|
47.1 |
58.2 |
58.1 |
|
|
Upper bound 2 |
|
44.5 |
56.7 |
56.9 |
|
|
|
Simulation |
21.7 |
43.6 |
54.4 |
55.8 |
57.8 |
|
|
100 |
Upper bound 1 |
|
54.1 |
56.8 |
61.9 |
|
|
Upper bound 2 |
|
53.4 |
56.4 |
61.4 |
|
|
|
Simulation |
26.3 |
52.1 |
55.3 |
60.3 |
60.3 |
4.10 Results Discussion
The simulation results (which include tissue type incompatibilities) are very similar to the theoretical upper bounds we develop in the case that only blood type incompatibilities are considered. While 2-way exchanges account for most of the potential gains from exchange, the number of patients who benefit from exchange significantly increases when three or more pair exchanges are allowed.
4.11 The Strategy of Patients
For each patient, we consider the best choice is to maximize the expect value of QALY (Quality Adjusted Life Year). We suggest using the risk decision-making method to decide whether to take an offered kidney, taking in account of the probabilities of each choice and status. However, due to lack of enough data, we are regretful to say that we cannot get any numerical results. In our future work, more things need to be done.
5. Political and Ethical Issues
5.1 Political Issues on the Transplant System
Nowadays, the OPTN contributes a great deal to the efficiency of various transplantations, and tens of thousands of patients gain benefits from the network. However, the OPTN still has a long way to go for its faultiness and lack of resources
The
regionalization of the OPTN raises the question that whether the transplants
should be performed in a few large centers and by a few experts or not. The
public calls for a fairer system.
We know
that the OPTN is divided into 11 regions in the whole nation. Each region
includes several states. Some Organ Procurement Organizations (OPO) are located
in the big cities of the state as well as the transplant center (TXC). The
transplantation surgeries are performed in the centers. In our opinion, there
are numerous reasons to support the idea of the OPTN organization. On one hand,
transplantation is, unlike others, a big surgery, which requires high standard
of either technology or environment. Only a few large centers in the big cities
can provide the basic necessities for the surgeons to perform a successful
transplantation. Research shows that big hospitals not only have a higher
survival rate of post-transplantations, but also give the recipients greater
confidence to accept this vital surgery. Who will consign his or her life to a
small hospital in a small community? On the other hand, all the kidneys donated
by the diseased are delivered to the center from the periphery. This creates
convenience for the OPTN to preserve and allocate the cadaver kidneys. By
contraries, if each kidney was kept in the hospital which is the nearest to the
diseased, it would increase the complexity and lower the efficiency of the
network or even let out a bedlam. In a word, carrying out the transplantation
in TXC will by no means harm the interest of the recipients.
However,
accomplishing the transplants in big hospital poses another question: Should
transplants be performed only by the expert surgeons? The answer is definitely
no. Everyone needs accumulated experiences to become an expert, and doctors are
not an exception. Assuming that all the chances are given to the most experienced
doctors who are minority, other less experienced doctors will be incapable of
making progress. When these experienced experts retire, who can take the place
for them? The transplant centers should cultivate young doctors for the
succession between generations. Some doctors live in the relatively small
community, where they have few opportunities to do transplants, since all the
kidneys are in the hospitals in metropolis. We suggest that the TXC can design
some plans to offer jobs in the big centers to the local doctors periodically.
In that way the proficiency of the doctors can be maintained.
We
believe that the OPTN is working at an increasing efficiency in the movement.
Although our goal is to make the system fairer, it should be bore in mind that the
completely fair system does not exist. What we are chasing for is the balance
between the equality and efficiency. Hence, we draw to the conclusion that it
is better to perform the transplant in big centers rather than in small
hospitals, while all the doctors should be provided the chance to gain
experience.
5.2 Ethical Issues in the Transplant System
Whether choosing an offered cadaver kidney
or waiting for a more compatible one from queue and exchange, patients in need
of organ may face dilemmas when they embark on the search for substitutes for
there body parts from deceased donors. On the grounds that there are brain
death and cardiac death donors, as well as standard and expanded donors, in the
scope of deceased donation, part of the case is the same as in that of living
donors, where there are remarkable ethical aspects to consider, e.g. the
recipients’ own health conditions, age, sex, ethnicity, financial status, etc.
Currently, relative patient waiting time plays a unique role in kidney allocation
in establishing fairness. The rise of kidney exchange is more or less a
consequential event of the waiting time inflicting most patients. An instance
is that to get on the list, according to policies, pediatric candidates (<
18 years old) begin accruing waiting time upon listing without their renal
condition considered which does for adults [OPTN 2005]. This may not seem
reasonable enough. Although children have longer life expectancy, medical
aspects should account for waiting time initiation, but maybe to a lesser
degree compared to adults. Still, ethical standards are not rigid doctrines; if
a patient is 18 years and 1 day old and needs a kidney much more deadly than a
17 years and 364 days old juvenile who has only mild symptoms, then it is us
that face an “agonizing choice”. Various forms of exchange program should be
promising to alleviate the issue of waiting time, and even accessibility.
Prevailing practice of transplant grafts in metropolises versus small towns is
determined by the rank order of patients on the local, regional, or national
lists of the allocation system; and the ultimate decision of organ accretion
and transplant graft resides with the liable surgeon or physician [OPTN 2005].
The geographical disparities following this can be averted through improved
allocation algorithm put into practice and organ quota interchange, providing
patients extra solutions. In legislature terms, “presumed consent” brings about
good paradigms in
5.3 The Discussion of Selling Organs
When it comes to living organ donation,
organ trade-off for transplantation exerts sensitive impacts on the community.
Most individuals, communities, and nations, with shared believes of the World
Health Organization and the Transplantation Society, say no because it’s
outrageous to think of human bodies as commodities. As far as we recognize,
organ transplant requires concern from and for the whole community, and
commercialization will not be applicable eventually when scarcity no longer
weakens the effectiveness and goal of organ transplant. Some Asian countries
legalize kidney trade to help close black market (like in
5.4 Reports to the Director
In this
report, we would like to give some recommendations to the transplant system in three
aspects, the political issues, the ethical concerns, and organ selling.
Currently,
organ transplant surgeries are performed only in a few large centers. We
consider it reasonable and beneficial. The hospital in the metropolis can
provide the doctors with more and better resource for transplantation, as well
as necessary diagnosis to the patients. Moreover, the donors in the centers are
under regular management. As a result, transplants should be performed only in
a few large centers. On the other hand, doctors in the small communities should
be offered sufficient opportunities to do the transplant surgeries, just as the
experts are. When the efficiency is maintained, fairness is ensured.
Criteria
is developed to determine whether a patient should be placed on the waiting
list or not, and to rank the priority of the candidates on the list. We try to
rank the criteria for priority and placement. First, there is no doubt that
patients with severe illnesses such as AIDS should not be placed on the list since
it is just a waste to transplant an organ to them, especially when available
organs are scarce. We rank the three main criteria used in determining priority
as follow: the quality of match, time on the waiting list, physical distance
between donors and recipients. The quality of match is the most important. If
patients accept kidneys which match them badly, they will face painful results:
to transplant again or keep using the unsuitable kidney, which causes a
decrease of the efficiency and effectiveness. Thanks to the success of chronic
dialysis, patients waiting for kidney transplant are generally not at the
immediate risk of dying. Thus, time of is not so important as the quality of
match. The physical distance between donors and recipients does not play a
critical role in the determining the priority for transportation is under
increasing development. One of the most concerned issues of ethic is the
priority given to pediatric patients. We don’t recommend emphasizing too much
on the priority of children. According to the data report of UNOS, the survival
rate varies not much between different age groups. 18 years old is a
controversial point. More research must be done to design a fairer policy for
the system concerning the age of recipients.
We are inclined
to forbid organ selling. Human bodies can not be considered as commodities.
Allowing the business of selling and buying organs will eventually become a
game among the wealthy. Though it may serve as an incentive bonus for donors,
the disadvantages greatly exceed the advantages. We can develop other methods
to recruit more donors, for example, improving the medical insurance system.
Donors can receive compensation after transplantation, tangible or intangible.
All in all, the interest of donors and recipients must be guaranteed, but not
by organ selling.
6. Recruiting more Donors
6.1 Factors Influencing Donation
Enduring
organ malfunctions is by no doubt a nightmare for anyone having it. When the
misfortune comes in the way of renal failure, huge amount of money would be
used for the medical treatment. Yet kidney dialyzes, though costly but a
necessary way for patients of early-stage kidney failure does no help in the
case of end-stage organ failure. As a result, a kidney transplant is recommended.
According
to the sorting access of various governments, people are considered as groups
of ‘presumed consent’ or ‘presumed discontent’. This sorting access takes its
place in defining the deceased donor but has nothing to do with live donor for
what we are now. Decease donor pool has quite a number of organs on the list,
but kidney shortage has never faded. So it is advocated that we healthy people
donate our kidneys when it is necessary. However, various factors contribute to
the shortage of live kidney donation.
Firstly,
pristine personal issues play the most important part. The fear of losing
organs may prevent most of people from donating. Losing one’s own organ is
always a nightmare to anybody. In fact, physical integrity may help to preserve
a sense of mental integrity just because it is something natural. As a matter
of fact, physical scathe is naturally common as crashes are always here and
there around our daily life. Yet an incision of organ would be quite another
affair. Few people would like to have their origin replaced unless an end-stage
organ failure is announced. Losing a precious part of the nature-given body for
not so evidenced private reasons may arouse affections of phobias; even
irrational fears that can finally make ships of hope take the ground. Hence, a
great level of altruism is recommended here. Under certain condition this willingness of dedication can be
greatly enhanced. For instance, in a relationship of relatives, siblings, or
even best friends, feeling of trust flourishes especially when life danger
comes up.
Secondly,
primary experience of medical treatment of the past will also have certain
impact on this issue. Kidney donating is quite serious and a highly perspicuous
understanding is recommended. Unfortunately not enough propaganda has been
promoted comparing to the severe shortage of kidney. Thus quite a lot of people
are held back from the queue of expected donors just because previous
displeasure experiences with surgery and regardless of the impendency of the
patients. In addition, many people are quite misinformed that kidney transplant
will harm a lot and even baffle people’s daily life.
Thirdly, rational consideration may have been taken but the answer may
be various and leads to different results. On the one hand, for those who care
more about the medical result of the recipient, the probability of success for
the recipient comes in the first. The fear should be cleared away for that
official data shows though considering various factors such as blood type, ethnicity,
age, gender and so on, patients accepting transplant still share high survival
rate which just differs from year length. Patients’ survival rate is totally
95.7% for male and 96.4% for female in the first year and it decreases as the
years accumulate until 84.4% for male and 85.9% for female in the fifth year
(OPTN 2007), and the probability of failure will be minimized if HLA matches
well and KPD was used. So the transplant can be
concluded to be safe. On the other hand, all expected donors will not miss himself/herself for risks are always there no
matter how good one’s physical condition is or how good the surgery is.
Obviously, the survival probability of the donor arouses the most attention.
Data shows that death from kidney donation is extremely rare (about
Yet
by no doubt the graft’s postoperative activities will be limited. One should
not lift anything heavier than 20 pounds for the first six weeks and may find
that frequent naps are needed for the first few weeks. But careful recuperation
will surely make a perfect one return.
In conclusion, a person can lead an active, normal life with only one
kidney. Studies have shown that one good kidney is enough to keep the body
healthy. After recovery from surgery, you can work, drive, exercise and
participate in sports as usual. You can continue in all types of occupations,
including military duty.
6.2 The larger the net, the bigger the mesh
Prolonging one’s relatives’ life
has always been the most positive motivity for potential donors to contribute
their organ, so a direct transplant to the relative or friend is quite
efficient and not to mention techniques in this CsA age.
While entering a list paired
network is quite another affair. The n-paired network divides all people in the
net into n pairs and recommends that each pair should exchange their kidney
nearly at the same time no matter whether the kidney is suitable or not. Hence
great risks exist here for the reason that a tiny malfunction of a kidney from
an individual in the net will lead to a total break down. Therefore potential
donors bear unexpected risks of kidney malfunction and the stranger feeling to
the recipient. Thus remarkable impact is caused and obviously the larger the n
is, the greater the risk is and less percentage of potential donors will donate
with consent.
6.3 Recommendations of recruiting more altruistic donors
To convince people to donate their precious
kidney, policies should be perspicuous to the public. Therefore, introduction
of organ transplant should be introduced into both school education and public
education to mitigate the effect of misinformation and enhance the altruism of
donation. Moreover, the survival rate, superior medical conditions of the
country and so on should be show to the public to convince people that kidney
donation would be fully guaranteed. Additionally, certain policies to encourage
possible donors should be put forward. Nowadays people who has a relative or so
who agrees to exchange will have the priority for transplant and this may have
most of its impact to relatives of the patients but not to any of those healthy
or wealthy families. Though here it is more a matter of "being forced
to" than "being willing to ", postoperative treatment for the
donor should be more human. In fact, providing financial aid is concluded as
the most human way for whoever the donor is. A recent survey indicates that as
many as 40 percent of potential kidney donors ultimately decide not to donate
due to financial concerns (UAB Media, 2006). Comparing with the value of a
kidney, we recommend that more welfare be given to the donors. Salaried
vacation after the operation can be introduced here, health insurance rate can
be lowered for them, regular medical exam can be taken as benefits, and the
psychotherapy is strongly recommended here since many donors may feel depressed
if they find out that they are not so vigorous as before so a vicious circle
may take place mentally and finally physically.
7. References
[1]Stefanos A.Zenios .1999.Evidence-based Organ Allocation.
[2]Alvin E.Roth.2006. Efficient Kidney Exchange: Coincidence of Wants in Markets with Compatibility-Based Preferencess
[3]Sarah E.Taranto.2002.Developing a national allocation model for cadaveric kidneys
[4]Robert A.Wolfe.2000.Comparison of moralilty in all patients on dialysis,patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant.
[5]Sundaram Hariharan.1996.Improved graft survival after renal transplantation in the united states,1988 to 1996.
[6]OPTN Evaluation Plan Updated on August 15,2005
[7]Xuanming Su.2004.Patient Choice in Kidney Allocation:The Role of the Queueing Discipline
[8]Xuanming Su.2004.Patient choice in kidney allocation: A sequential stochastic assignment model
[9] Christian Jacquelinet1 MD PhD,Changing.2004.Kidney Allocation Policy in France: the Value of Simulation.
[10] Juan J. Abellán.1998.PREDICTING THE BEHAVIOUR OF THE RENAL TRANSPLANT WAITING LIST IN THE PAÍS VALENCIÀ (SPAIN) USING SIMULATION MODELING.
[11] Gert Mayer1,Eurotransplant kidney allocation system (ETKAS):rationale and implementation
[12] Susan Fuggle,.1999.National Kidney Allocation in the UK - Issues for Histocompatibility and Immunogenetics Laboratories
[13] Sommer E. Gentrya,.1999.A Comparison of Populations Served by Kidney PairedDonation and List Paired Donation